Christmas Day, the kids and I all piled into the car to drive into Philadelphia to visit George. I made a Christmas brunch so we could open gifts and eat early, then spend the rest of the day with George.
We left the house at around 1:00. As I was getting ready to turn into the parking garage, my phone rang and it was a Philadelphia number, so I answered immediately. It was someone at the hospital calling to tell me that they had to call the Rapid Response Team into George’s room because he had an incident. I’m not going to lie…I can not remember what that woman said. I couldn’t grasp what I was hearing. I told her we were pulling into the garage and she said she would meet me at the door to George’s room.
When we got to George’s room, it was all abuzz…there were so many health care professionals around the outside, and on the inside. The woman I talked to on the phone approached me. She told me that George had tried to make his way to the bathroom to have a bowel movement, but didn’t make it and had to call the nurse by pulling the string next to the toilet for help. His stool was like “pudding” and had dark blood in it. And he also had bright red blood running down his leg. He couldn’t breathe and was scared. He was losing a lot of blood.
When I went into the room, they were working hard to stabilize him. I stood at the foot of the bed and he saw me and started crying. He looked so scared and overwhelmed.
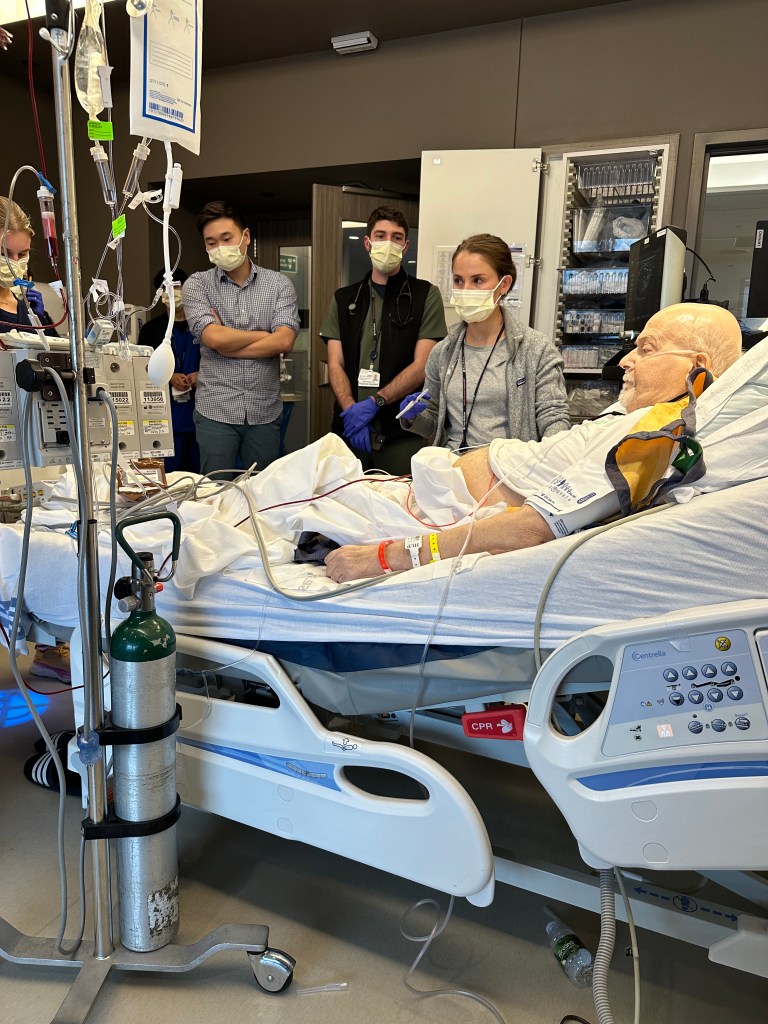
They wanted to put a catheter in his jugular vein which was thicker and would allow a faster transfusion than the PICC line in his arm. He was given 12 units of blood and 12 units of platelets. That’s A LOT!
Once the RRT got him stabilized, he was transferred to the ICU on the 14th floor. They suspected an abdominal bleed, so they also wanted to do an endoscopy of his upper GI to see if there was something going on there. First, they inserted the catheter into his jugular. I had to leave the room while they did that. Then we all were allowed in before they sedated him for the endoscopy. He was also put on a ventilator, which I knew scared George, but the doctor said he was ok with it because they told him it was temporary.
They did the scope and afterwards, we were allowed into his room. He was still sedated and on the ventilator.

I asked the NP, Molly if he was going to stay like that all night and she said yes. I guess they wanted him to be ready in case another emergency occurred overnight. She asked me to sign a consent to insert another catheter if they needed to so they wouldn’t have to call me in the middle of the night, so I did. She told us to go home and get some rest, so we did. Before that, I did have a chance to talk to the gastrointestinal doctor and he said they saw no blood in his upper GI. He said he was surprised! So – that was not the site of his bleeding.
The next morning, I called the ICU floor and talked with George’s awesome nurse, Tom. He said George was doing well and was off the sedation and communicating with them using a dry erase board. They planned to remove the breathing tube later in the morning. So, we all got ready and went up to visit George again. He looked much improved! No more tube! We had a nice visit with him, although he was distracted by the premier league soccer on the television.
Current situation: I went to see him today (Dec 27th)
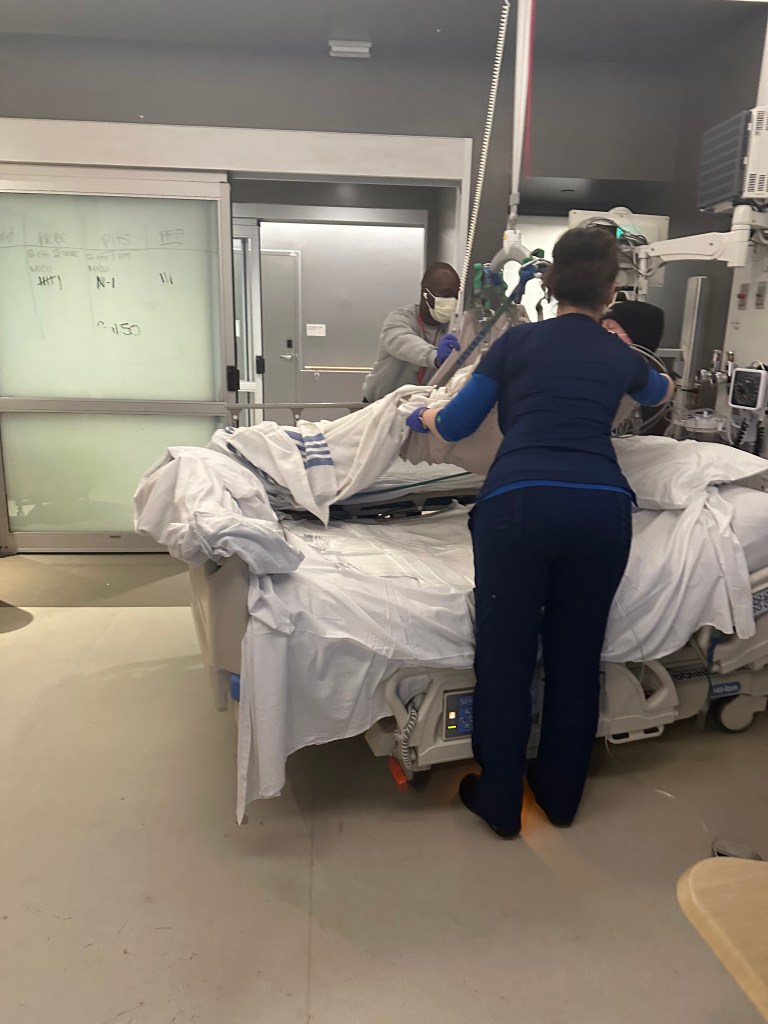
-George can’t stand or walk on his own. His legs are so thin and weak due to the atrophy of all his muscle tissue. This means he isn’t allowed to walk to the bathroom and has to use a bedpan and urinal. He hates that! He DID have a foley catheter, but the nurse took that out this afternoon. When he went down to have a CT scan done of his chest today, he was transported on a gurney and when he returned to the room, they used the “lift” to move him from the gurney to the bed, which looks like a basket or something hanging from the ceiling.
– His feet and ankles are swollen.
– He struggles to move/ sit up in his bed because his arms are so weak, he can’t push himself up very well.
-He is on 4 liters of oxygen
-He started coughing today – sounds like some stuff in his lungs. They did a CT scan of his chest today and then told him they needed to do a COVID/flu/RSV swab because they said it looked as if he had some “stuff” in his lungs.
-George’s blood cultured positive for bacteria. Enterobacteriaceae and staph to be exact. Because the enterobacteria can be resistant to antibiotics, we now have to wear yellow gowns while in his room and take them off before leaving so we don’t carry the germs out onto the floor and possibly to other patients’ rooms.

-The doctor asked if he had any pain or tenderness on his right side. He said not really. So, she pushed on his side and he winced. She said they saw inflammation of his gallbladder and “sludge” and weren’t sure what it was. So, they are thinking it could be from the bacteria. They are keeping an eye on that. Hopefully the antibiotics he is taking will fix that right up. We’ll see.
Was it really just a few days ago, he was working at his desk and walking down the hall and to the bathroom?

I feel like so much has happened over the past 48 hours and I may have left something out. It’s overwhelming for both George and me.
He is scared….today he asked me, in tears, if he is going to die. Before I could answer, he said “Don’t tell me. I don’t want to know. I’m not going to let that happen.”
I will update you when we get more news/ results or, God willing, progress.

Leave a comment