In my last post, I wrote that we are moving towards a second bone marrow transplant and that there is a delay because of the results of George’s bone marrow biopsy: he had too many blasts (immature white blood cells). So, on Wednesday, we met with Dr. Loren to discuss the results and plan our next steps.
The first thing she said was that the clinical trial was full until September, so that kind of settled that question. They can only do one patient per month and both July and August were taken. She said she may talk to her colleague about removing George’s T-cells and freezing them and then using them in September. I don’t know. A lot of this stuff is above my pay grade and all I can do is try my best to understand and then convey it here.
She then moved on to George’s biopsy results. She said what we already knew…chances for the bone marrow transplant working/ lasting are increased if the patient is in remission. So, George started a round of chemo on Monday to hopefully get him into remission. Actually, it is essential he be in remission at transplant. Turns out he has 23% blasts and anything over 20% is leukemia. He will do the standard regimen of venetoclax and azacitadine, which he has done several times before. He will go in for 7 days in a row for the infusion and then keep taking the pill for a total of 21 days. The azacitidine is the drug that the doctors suspected cause George’s lung issues that landed him in the hospital, but since the pulmonologist is confident that he was suffering from post-COVID organizing pneumonia and not drug damage, we are going back to what we know works. Then George will go in for a bone marrow biopsy on August 4th and we will meet again with Dr. Loren on the 9th to discuss the results. If all goes as planned, George will have his transplant around the 3rd week of August.
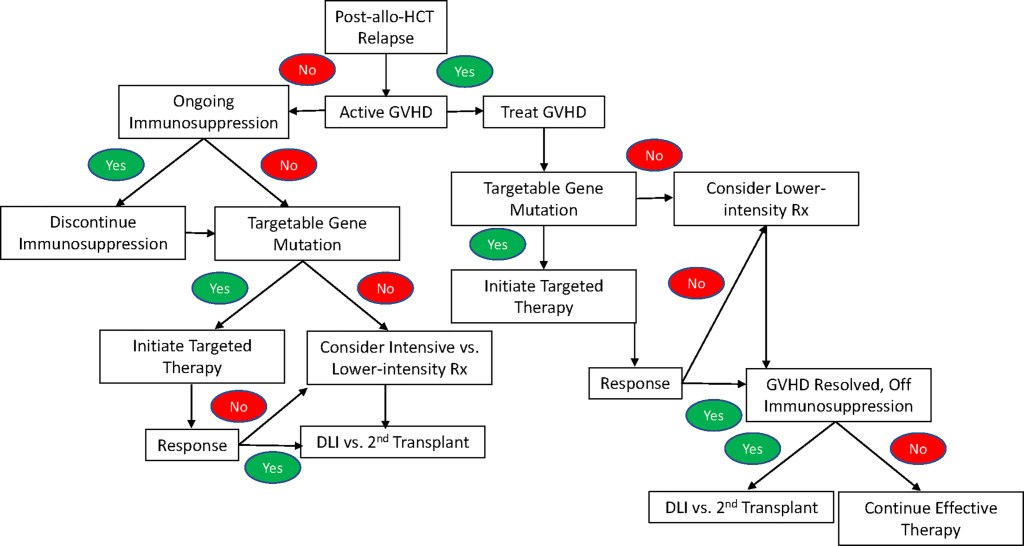
How we decide the next steps after post-transplant relapse:
George has done targeted therapy for his FLT3 mutation and amazingly, the mutation was gone when we looked at the results of his bone marrow biopsy he had in April. But then, of course he gained new ones… mainly the freakish deletion of the long arm of his 7th chromosome.
After some discussion, I asked Dr. Loren a question. I said, “George and I had been discussing the fact that when he was first diagnosed, he was told that it was very desirable to have his bone marrow transplant during his first remission. Where does that put George right now?”
She nodded her head while I was speaking and then said, yes…the odds of success are greater during that time. So, George is facing some new challenges this go round.
According to what I have found on credible sources on the internet, the prognosis of patients after repeat bone marrow transplantation depends primarily on the length of time between first remission and relapse. On average, the survival rate among patients with less than a year of remission is HALF that of those whose remission lasted longer. (George’s lasted 6 months).
That is definitely something that makes you catch your breath, no doubt. I don’t want to ask Dr. Loren to clarify or explain it in front of George because he needs to stay positive and not be demoralized. I don’t share my findings on the internet with him either. He does not seek out information online and I have to believe it’s because he doesn’t want to know and also, I have seen his reaction when I have done so in the past. Obviously, he doesn’t read my blog either!
There are a couple of other things that will make this transplant more challenging. First, George, as a second BMT patient, will enter treatment in a weakened state after previous courses of chemo and radiation, so physicians use a mitigated approach. This is called reduced-intensity conditioning – using lower doses of chemotherapy and radiation therapy in preparation for the patient’s BMT. This approach is less toxic to the body, but has a higher risk of relapse. Pretty discouraging as he relapsed after the intense conditioning regime.
Dr. Loren said his mutations, like ASXL1 and the missing long arm of his 7th chromosome also affect his prognosis negatively. Let’s take a look at all the unfavorables George has going on:

Again….not sure how this information carries through transplant. In other words, are these negative markers an indication for the need for a transplant – a deciding factor whether or not to transplant and transplant will take care of them? I want to ask Dr. Loren, but will have to wait until Aug 4 I guess.
Dr. Loren also said that George’s leukemia is stubborn and aggressive (because of all the negatives listed above), which is another challenge to overcome, especially since he can’t have the strong, myeloablative chemo and radiation before transplant.
But, George does have some strengths going into this thing! First, he is still considered “young” in the leukemia world. Under 60 is young and George is 59. So, that’s favorable! Secondly, he is in good shape – feels good, good appetite, walks 3-4 miles on the weekends, and is working full time in his home office. Another check in the plus column.
So, now we have a good idea of the challenges that lies ahead and George is ready to get started. Challenge accepted. But to say it’s not scary would be a lie.

Leave a comment